Asia’s economic progress continues amidst global economic downturns. Estimates suggest the region’s economy will expand by 4.8% in 2024. This growth stems from strong domestic consumption, rising exports, and a resurgence in tourism. However, this economic upswing sharply contrasts with the demographic reality of a rapidly aging population, projected to reach nearly 923 million individuals by 2050.
You Can Also Read: UNIVERSAL PENSION SCHEME: THE FIRST STEP TOWARDS A WELFARE STATE
These figures present significant hurdles, as current healthcare and pension systems lack adequate preparation to support this burgeoning elderly demographic, especially in rural areas where infrastructure lags. Addressing this gap between economic success and the well-being of the aging population requires innovative policies and increased investment in elderly care services.
Challenges Faced by the Elderly
The aging population in Asia faces a multitude of challenges, many of which are interrelated and mutually reinforcing. Access to quality healthcare remains a pressing issue, with rural areas often lacking adequate facilities and personnel.

This healthcare deficit is compounded by financial constraints, as many elderly individuals lack sufficient savings or pensions to cover medical expenses. There are four reasons why current pension systems are unlikely to deliver a secure income in old age:
- The extent to which formal pension plans are utilized is quite limited.
- It’s a frequent occurrence for individuals to access their retirement funds prematurely.
- There’s a tendency for retirees to receive their pension savings in one go, which poses the danger of depleting their funds before the end of their life.
- The amount of pension received does not regularly increase to compensate for the rising cost of living.
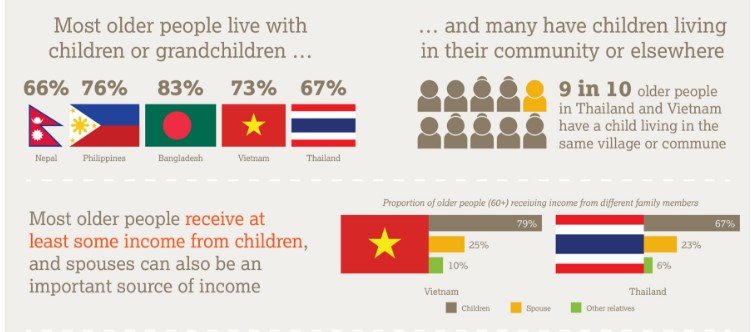
Furthermore, the traditional family support system is eroding due to urbanization and changing societal norms. The erosion of the traditional family support system is influenced by a variety of factors, particularly in urban settings. Here are some key factors contributing to this trend:
- Urbanization: As people move to cities for employment opportunities, the joint family system, which is characterized by multi-generational living arrangements, is being replaced by nuclear families.
- Socio-Economic Changes: Increased education, career opportunities, and exposure to globalized values have led families to prefer smaller, more independent units.
- Cultural Shifts: There’s a transformation in family ideals and aspirations, influenced by globalized values and cultural shifts towards individualism.
- Demographic Changes: The rise in single-parent families, cohabitation, same-sex families, and voluntary childlessness are changing the nature of families.
- Economic Factors: Changes in the economic structure, such as the inability to support a nuclear family on a single wage, have impacted family life and the support system.
Consequently, an increasing number of elderly individuals find themselves living alone or in institutional care settings, which can exacerbate feelings of isolation and loneliness.
Economic Progress and Demographic Shifts
Asia’s developing economies are projected to experience a 4.8% growth rate in both 2023 and 2024. This expansion is fueled by robust domestic consumption, improved exports of semiconductors, and the ongoing revival of the tourism industry. Despite global challenges, including the Russian invasion of Ukraine impacting commodity prices, the region’s economic outlook remains optimistic.
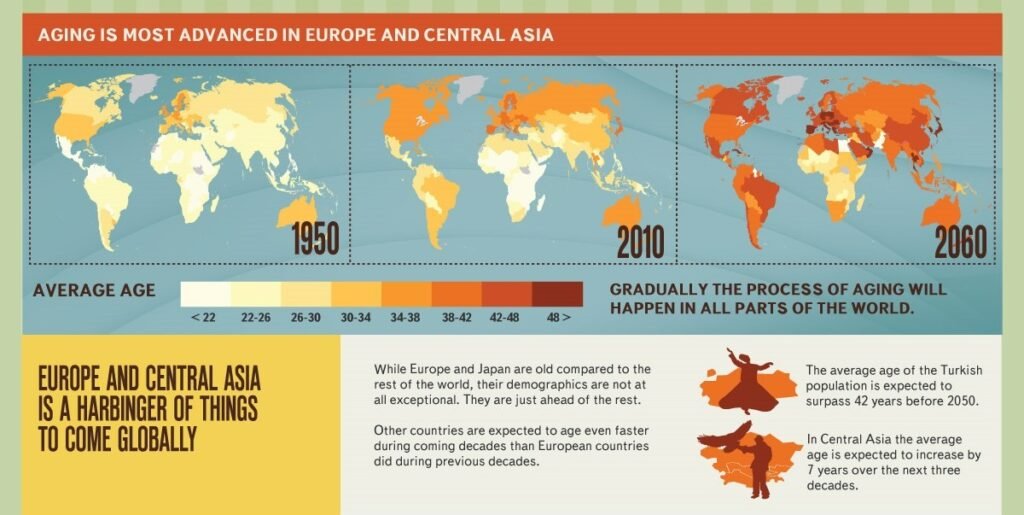
Concurrently, Asia is witnessing a significant demographic shift, with estimates suggesting that the elderly population will reach nearly 923 million individuals by the year 2050. This rapid aging of the population presents new hurdles for the region, as the current infrastructure, particularly in the healthcare and pension sectors, may not be adequately prepared to support this demographic transition.

While Asia’s economies demonstrate resilience, the pressing need to enhance support systems for the aging population highlights a critical area that demands focused policy attention and increased investment.
Long-Term Care: A Growing Necessity
Across Asia’s developing nations, the rapid aging of the population is driving an escalating demand for long-term care services. By 2050, the number of elderly individuals in the region is expected to surge, significantly increasing the need for various long-term care options. Types of long-term care services that can help people live as independently and safely as possible when they can no longer perform everyday activities on their own are:
Home-Based Care:
- Informal Caregivers
- Formal Caregivers
- Community and Residential Care
- Adult Day Care Centers
- Assisted Living Facilities
- Skilled Nursing Facilities (Nursing Homes)
- Memory Care Units
- Continuing Care Retirement Communities
- Board and Care Homes
Other Options:
Retirement Living/Independent Living: Communities designed for active seniors who want to downsize and enjoy social activities.
Medical Foster Care: A home-based program where trained caregivers provide care for individuals with medical needs.
At present, many Asian countries are grappling with substantial gaps in the provision of long-term care.
Population Aging and Health Burden: Rapidly Aging Population Over the past two decades, life expectancy at age 60 has increased by more than 5 years in the region.
Noncommunicable Diseases (NCDs): On average, 57% of Asians aged over 60 have at least one diagnosed NCD. This share varies across countries, ranging from 35% in Bangladesh to 68% in the People’s Republic of China.
Mental Health Issues: Almost one-in-three older persons in Asia and the Pacific report depressive symptoms.
Challenges in Long-Term Care:
Functional Impairment: The average share of older people reporting functional impairment in at least one primary activity of daily living (ADL) stands at 20.
Care Gaps: On average, 43% of older Asians with functional limitations experience care gaps.
Efforts are underway to improve the situation, with initiatives focusing on expanding access to care and enhancing the quality of services. The World Health Organization emphasizes the importance of establishing long-term care as an integral part of universal health coverage, building a sustainable workforce, and ensuring a high standards of care quality. These efforts include providing technical support for national care strategies and designing tools for a minimum care package, which also considers the needs of informal caregivers.
Conclusion
Asia’s developing nations face an urgent need for innovative solutions to ensure the well-being of their rapidly aging populations. The region must accelerate the development of comprehensive long-term care systems that are accessible and affordable to meet the growing demand. Countries like India and Thailand are already crafting policies focused on improving health infrastructure and community-based care to support their aging populations.
Policymakers are encouraged to prioritize investments in healthcare facilities and services that cater specifically to the elderly. This includes enhancing the capacity of long-term care facilities and expanding coverage to include more of the aging population. Furthermore, community-based models are highlighted as sustainable solutions that can deliver quality services in low-income settings, supporting a larger share of the elderly population.
For Asia’s developing nations, the key to successful aging policy lies in integrated care strategies that involve government, private sector, and community efforts. These strategies should focus on strengthening the infrastructure and workforce needed to provide continuous care, while also utilizing technology to enhance service delivery and accessibility.
The region’s approach to elderly care is a critical factor of its broader social and economic policy framework. As such, the integration of health services into comprehensive social support systems will be crucial for fostering a dignified quality of life for all seniors in Asia.


