While maternal mortality rates have decreased by a third in the past 20 years, a woman still loses her life every two minutes because of complications during pregnancy or childbirth. A global report published by World Health Organization on behalf of the United Nations Maternal Mortality Estimation Inter-Agency Group comprising of different agencies of the UN has found that pregnancy related death is still a major mortality factor.
YOU CAN ALSO READ: WHY HEALTHCARE COSTS ARE RISING FOR INDIVIDUALS AND DECLINING FOR GOVERNMENT?
The Maternal Mortality Ratio (MMR) is the number of women who die from pregnancy-related causes during pregnancy or within 42 days of termination of pregnancy per 100,000 live births. In 2020, around 287 000 women died during pregnancy and after childbirth. Preventable maternal mortality accounted for about 95% of all deaths in 2020, with the vast majority occurring in low and lower middle-income countries.
Region-wise maternal mortality ratio around the world
Sub-Saharan Africa alone was responsible for around 70% of maternal mortality, while Southern Asia was liable for about 16%. Between 2000 and 2020, Eastern Europe and Southern Asia saw the biggest drop in maternal mortality ratio (MMR): 70% and 67%, respectively. Sub-Saharan Africa had an extremely high MMR in 2020, yet the region also successfully reduced its MMR by 33% between 2000 and 2020. Over this period, four SDG sub regions approximately halved their MMRs: Eastern Africa, Central Asia, Eastern Asia, and Northern Africa while Western Europe lowered their MMRs by approximately one-third.
Overall, the maternal mortality ratio (MMR) in the world’s least developed nations decreased by just under fifty percent. The MMR reduced by 50% in landlocked developing nations. The MMR fell by 19% in small island developing countries.

Reduced maternal mortality ratio
According to a report by the World Health Organization and other UN organizations, the global maternal mortality rate decreased 34.3% over a 20-year period, from 339 maternal deaths per 100,000 live births in 2000 to 223 maternal deaths in 2020. That still equates to almost one woman dying every two minutes in 2020, or nearly 800 women each day.
Where are the maternal death rate high?
Maternal deaths continue to be disproportionately concentrated in the world’s poorest regions and conflict-affected nations. Around 70% of all maternal deaths in 2020 occurred in sub-Saharan Africa. The maternal mortality rate was more than double the worldwide average in nine nations experiencing severe humanitarian crises (551 maternal deaths per 100 000 live births, compared to 223 globally). The countries are -Afghanistan, the Central African Republic, Chad, the Democratic Republic of Congo, Somalia, South Sudan, Sudan, Syria and Yemen.
Bangladesh’s maternal mortality rate and SDG 3
Bangladesh has made tremendous progress in reducing maternal death rates over the past five decades, achieving the top spot in South Asia last year.
According to the Ministry of Health and Family Welfare in Bangladesh, the rate of maternal mortality in 2009 was 269 per every 100,000 births. The ratio has dropped to 62.3 in 2022. The government’s goal is to minimize maternal mortality to less than 50 per 100,000 live births.
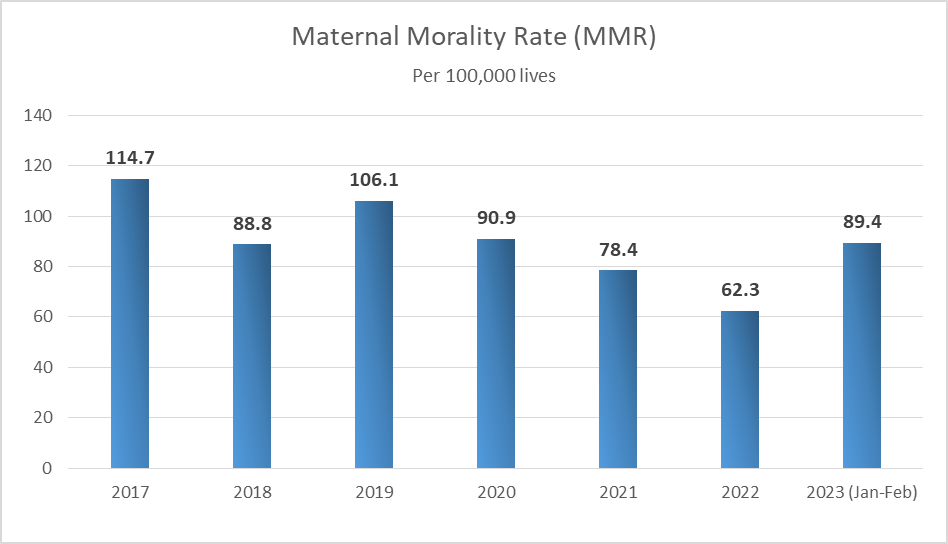
According to the Directorate General of Health Services (DGHS), the maternal mortality rate decreased from 114.7 per 100,000 in 2017 to 62.3 per 100,000 in 2022.
Division wise MMR in Bangladesh
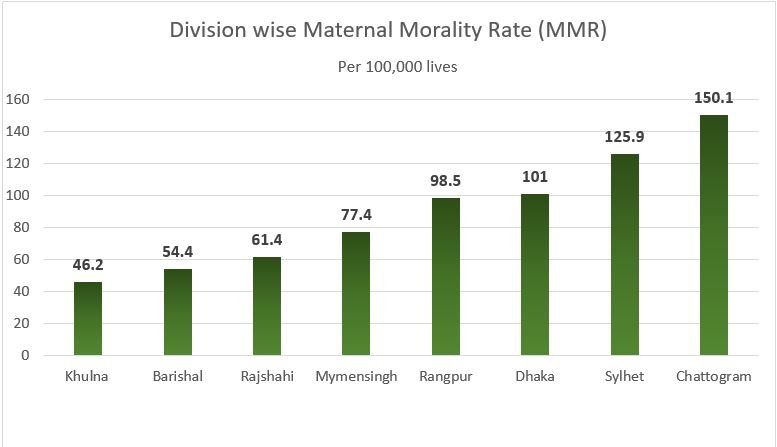
Out of the 8 divisions in Bangladesh, Khulna division tops with the lowest MMR of 46.2 out of per 100,000 lives. Chattogram division has the highest MMR of 150.1. The capital has the MMR of 101 (per100,000 lives).
With a global target of 70 per 100,00 live births established by SDG 3, Bangladesh has a lot of work to do to bring down the maternal death rate. Matiur Rahman, assistant director of the Family Planning Directorate, stated that 3,364 union health and family welfare centres provide maternal and child health care in addition to family planning services.
Experts say that in the 51 years since Bangladesh’s independence, the country has made extraordinary progress on every single health indicator.
Why maternal deaths occur? What can be done?
The primary causes of maternal mortality are severe bleeding, high blood pressure, pregnancy-related infections, complications from unsafe abortions, and underlying illnesses (such as HIV/AIDS and malaria) that can be exacerbated by pregnancy. All of these are substantially preventable and treatable with access to respectful, high-quality healthcare.
Community-centered primary health care can fulfill the needs of women, children, and adolescents and provide equitable access to vital services such as assisted deliveries, prenatal and postnatal care, childhood vaccines, nutrition, and family planning. Yet, underfunding of primary health care systems, a lack of qualified health care professionals, and inadequate supply networks for medicinal supplies impede progress.
About a third of women don’t get even four of the recommended eight prenatal checks or the care they need after giving birth, and about 270 million women don’t have access to modern methods of birth control globally. Inequalities in income, education, race, or ethnicity increase the risks for marginalized pregnant women, who have the least access to essential maternity care and are most likely to have health problems during pregnancy.
Women need to have control over their reproductive health, especially when and if they want to have children. This is important so that they can plan and space out their pregnancies, protect their health and life.


